Table of Contents
ToggleIntroduction:
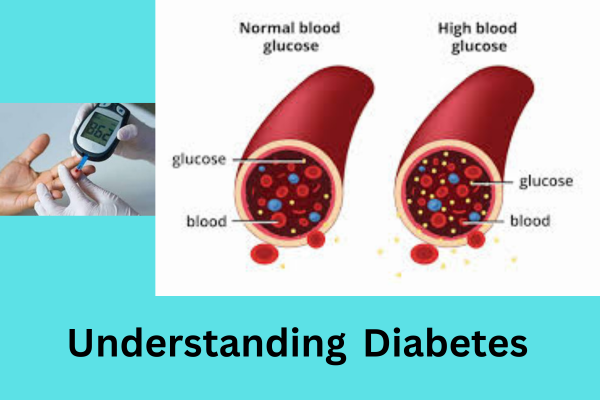
Diabetes mellitus, commonly known as diabetes, is a chronic metabolic disorder characterized by high blood sugar levels. This condition occurs when the body either does not produce enough insulin or cannot effectively use the insulin it produces. Insulin is a hormone produced by the pancreas, and it plays an important role in regulating blood sugar (glucose) levels, allowing cells to use glucose for energy.
Historical Context:
The history of diabetes goes back thousands of years, with the earliest descriptions of the disease being found in ancient texts. However, the 20th century saw significant advances in the understanding of diabetes. The discovery of insulin by Frederick Banting and Charles Best in 1921 revolutionized the treatment of diabetes, saving countless lives. Since then, research has steadily increased our knowledge of diabetes, leading to improvements in diagnostic methods, treatment options, and diabetes management techniques.

Diabetes Awareness:
Diabetes is a chronic condition that can lead to death if left untreated. Known as the silent killer, it affects the body’s organ systems and can cause various diseases. For this reason, there is a need to spread knowledge about the disease. The recent World Diabetes Day, observed on November 14, aims to raise awareness of diabetes worldwide, encourage better care and support for people with the disease, and increase public understanding of diabetes. Intends to increase. Frequent medical check-ups that measure blood sugar levels make it easier to detect pre-diabetes and start early treatment.
Types of Diabetes:
Type 1 Diabetes:
Type 1 diabetes, also known as juvenile diabetes or insulin-dependent diabetes, is a chronic autoimmune condition where the body’s immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. Is. Insulin is the hormone needed to regulate blood sugar (glucose) levels, allowing cells to absorb and use glucose for energy. Without insulin, glucose accumulates in the bloodstream, causing high blood sugar levels and various complications.
Causes:
The exact cause of type 1 diabetes is not fully understood, but it is believed to involve a combination of genetic and environmental factors. People with a family history of type 1 diabetes are at higher risk. Additionally, certain environmental triggers, such as viral infections, can trigger autoimmunity in genetically susceptible individuals. Once activated, the immune system attacks and destroys the insulin-producing cells in the pancreas, leading to insulin deficiency in the body.
Symptoms:
Type 1 diabetes often develops quickly, and symptoms can be severe. Common signs and symptoms include:
Excessive thirst: increased thirst and frequent drinking of water.
Frequent urination: Excessive urination, especially at night.
Extreme hunger: persistent hunger even after eating.
Unexplained weight loss: Despite an increased appetite, people with type 1 diabetes may lose weight.
Fatigue: Feeling tired and lethargic.
Irritability: Sudden mood changes and irritability.
Blurred vision: Vision problems due to high blood sugar.
If left untreated, type 1 diabetes can lead to a life-threatening condition called diabetic ketoacidosis (DKA), which is characterized by a build-up of acidic ketones in the blood, causing dehydration, vomiting and diarrhea. Eventually coma occurs.
Diagnosis:
Diagnosing type 1 diabetes usually involves blood tests to measure blood sugar levels. Additionally, tests to detect the presence of specific antibodies associated with autoimmune diabetes, such as anti-GAD antibodies, can confirm the autoimmune nature of the condition.
Management:
Type 2 diabetes is a chronic metabolic disorder characterized by high blood sugar levels (hyperglycemia) that result from the body’s inability to use insulin effectively or insufficient insulin production. Insulin is a hormone produced by the pancreas that helps regulate blood sugar (glucose) levels and allows cells to use glucose for energy.
In people with type 2 diabetes, the body’s cells become resistant to the effects of insulin, meaning they do not respond properly to insulin, or the pancreas does not produce enough insulin to maintain normal blood sugar levels. This leads to the accumulation of glucose in the blood, which increases blood sugar levels.
Type 2 Diabetes:
Several factors contribute to the development of type 2 diabetes, including:
Genetics: A family history of diabetes can increase the risk of developing type 2 diabetes.
Obesity: Excess body weight, especially around the abdomen, is a significant risk factor.
Lifestyle factors: Poor diet, lack of physical activity, and unhealthy lifestyle choices can contribute to the development of type 2 diabetes.
Insulin resistance: As people age, their cells can become less responsive to insulin, increasing the risk of diabetes.
Metabolic syndrome: This cluster of conditions, including high blood pressure, high cholesterol, and insulin resistance, often precedes the development of type 2 diabetes.
Causes:
Type 2 diabetes is a chronic metabolic disorder characterized by high blood sugar levels (hyperglycemia) that result from the body’s inability to use insulin effectively or insufficient insulin production. Insulin is a hormone produced by the pancreas that helps regulate blood sugar (glucose) levels and allows cells to use glucose for energy.
In people with type 2 diabetes, the body’s cells become resistant to the effects of insulin, meaning they do not respond properly to insulin, or the pancreas does not produce enough insulin to maintain normal blood sugar levels. This leads to the accumulation of glucose in the blood, which increases blood sugar levels.
Symptoms:
Common symptoms of type 2 diabetes include increased thirst, frequent urination, weight loss, fatigue, blurred vision, and slow healing. However, some people with type 2 diabetes may not have noticeable symptoms, which is why regular checkups and blood sugar monitoring are so important for early detection.
Management:
Management of type 2 diabetes usually involves lifestyle changes such as adopting a healthy diet, regular physical activity, and weight management. In some cases, oral medications or insulin therapy may be prescribed to help control blood sugar levels. Monitoring blood sugar levels, maintaining a healthy lifestyle, and working with health care providers can help manage type 2 diabetes and prevent complications such as heart disease, kidney damage, and neurological problems.
Gestational Diabetes:
Gestational diabetes mellitus (GDM) is a form of diabetes that develops during pregnancy, specifically affecting how the body handles glucose. This condition poses risks to both mother and baby and requires careful monitoring and management. Gestational diabetes usually appears in the second trimester and can lead to complications during pregnancy and childbirth if left untreated.
Causes:
The exact cause of gestational diabetes is not fully understood, but hormonal changes during pregnancy contribute to insulin resistance. Insulin resistance occurs when the body’s cells don’t respond effectively to insulin, causing blood sugar levels to rise. Because the placenta produces hormones that can impair insulin action, the pancreas may struggle to produce enough insulin to overcome this resistance, resulting in gestational diabetes.
Risk Factors:
Several factors increase the risk of gestational diabetes:
Age: Women over the age of 25 are at higher risk.
Family history: A family history of diabetes.
Race: Certain racial groups, including African Americans, Hispanics, Native Americans, and Asians, are more vulnerable.
Obesity: Being overweight before pregnancy increases the risk.
Previous Gestational Diabetes: Women who have had gestational diabetes in a previous pregnancy have a higher risk in subsequent pregnancies.

Symptoms:
Gestational diabetes often does not cause noticeable symptoms. However, some women may experience:
Increased thirst and urination: Like other types of diabetes, gestational diabetes can cause increased thirst and more frequent urination.
Fatigue: Feeling more tired than usual.
Blurred vision: High blood sugar causes changes in vision.
Complications:
If left uncontrolled, gestational diabetes can lead to various complications:
Preeclampsia: High blood pressure that can affect both mother and baby.
Macrosomia: Excessive fetal growth, increased risk of birth injuries.
Premature birth: Gestational diabetes can lead to premature birth.
Risk of type 2 diabetes: Women who develop diabetes during pregnancy have an increased risk of developing type 2 diabetes later in life.
Respiratory Distress Syndrome: Babies born to mothers with gestational diabetes may experience respiratory problems.
appraisal:
Gestational diabetes is usually diagnosed between the 24th and 28th weeks of pregnancy through an oral glucose tolerance test (OGTT). The test involves fasting overnight and then drinking a sugar solution before measuring blood sugar levels at specific intervals.
Management:
Management of gestational diabetes includes lifestyle changes and in some cases medications:
Healthy Diet: A balanced diet with carbohydrate control is very important.
Regular exercise: Moderate physical activity can help control blood sugar levels.
Blood sugar monitoring: Regular monitoring helps track and manage glucose levels.
Insulin or medications: In some cases, insulin or oral medications may be prescribed to manage blood sugar levels.
Postpartum Considerations:
After the baby is born, blood sugar levels usually return to normal. However, women who develop gestational diabetes should have regular checkups and screenings for type 2 diabetes.
Gestational diabetes requires careful monitoring and management to ensure the health of both mother and baby. With appropriate medical care, lifestyle adjustments, and postpartum follow-up, women with gestational diabetes can reduce their risk of complications and contribute to the overall health of themselves and their newborns.
Dietary Guidelines for the Management of Diabetes:

For people with diabetes, maintaining a healthy and balanced diet is an important aspect of managing blood sugar levels and preventing complications. Making the right dietary choices can play an important role in overall health and wellness. Here are the key principles and guidelines for designing an optimal diet for people with diabetes.
1. Carbohydrate Management:
Focus on complex carbohydrates: Choose whole grains, beans, fruits, and vegetables as your primary sources of carbohydrates. These foods contain fiber, which helps control blood sugar levels.
Portion control: Pay attention to portion sizes to avoid blood sugar spikes. Carbohydrate counting can be a useful strategy for managing intake.
2. Protein intake:
Choose lean protein: Choose lean sources of protein such as poultry, fish, tofu, beans and low-fat dairy products.
Balanced distribution: Spread protein intake evenly throughout the day to help keep blood sugar levels stable.
3. Healthy Fats:
Choose unsaturated fats: Include sources of unsaturated fats, such as olive oil, avocados, nuts and seeds, which can have positive effects on heart health.
Limit saturated and trans fats: Reduce the amount of saturated and trans fats, which are found in fried foods, processed snacks and some animal products.
4. Foods rich in fiber:
Add fiber: Fiber-rich foods, including whole grains, vegetables, fruits and beans, can help stabilize blood sugar levels and promote digestive health.
5. Glycemic Index Considerations:
Understand the glycemic index: Be aware of the glycemic index (GI) of foods. Choosing low GI foods can help manage blood sugar more effectively.
Combine meals: Combining carbohydrates with protein or healthy fats can help reduce the impact on blood sugar levels.
6. Regular Meal Time:
Consistent meal schedule: Eating regularly throughout the day can help control blood sugar levels. Avoid skipping meals to prevent extreme fluctuations.
7. Hydration:
Water as the primary beverage: Choose water as the primary beverage, and limit sugary drinks and excessive caffeine.
Moderate alcohol consumption: If alcohol is consumed, do so in moderation and with food to prevent hypoglycemia.
8. Individual approach:
Personalized meal plans: Work with a registered dietitian or health care professional to develop a personalized meal plan based on individual needs, preferences and lifestyle.
Monitoring and adjusting: Monitor blood sugar levels regularly and adjust dosage accordingly in consultation with healthcare providers.
9. Considerations for Weight Management:
Calorie Intake: For those who want to lose or maintain weight, monitoring calorie intake is important. However, extreme calorie restriction should be avoided.
10. Reading Food Labels:
Understanding labels: Learn to read and interpret food labels, paying attention to total carbohydrates, fiber and serving size.
A well-planned and individualized diet is the foundation of effective diabetes management. By adopting a balanced and mindful approach to food choices, people with diabetes can keep blood sugar levels stable, prevent complications, and improve overall health and quality of life. Regular communication with health care professionals, including registered dietitians, is important for ongoing guidance and support in navigating dietary considerations for diabetes.